Celebrating 100 Years of Commitment to the Carolinas
January 18, 2024 | Eric E. Frazier
The Duke Endowment was established a century ago by James B. Duke and continues to be inspired by the people of the Carolinas and a shared vision for our future.
A Century of Intentional Support in Pursuit of Shared Opportunities in Higher Education
February 28, 2024 | Kristi K. Walters
The Endowment's Director of Higher Education reflects on a century of support for the four institutions of higher learning named in our founder's philanthropic mandate.
Latest News & Stories
Get the latest from the Endowment and read more about the impact of the work being done by our grantees and individuals in the field

Former Church Buildings Find New Purpose
Congregations are banding together to repurpose empty churches as community pillars to address issues like housing.
February 14, 2024 | Public News Service

Make Giving and Getting Help Easier for Families and Caregivers
February is Family Support Awareness Month.
January 31, 2024 | Phillip H. Redmond Jr.
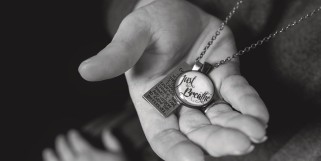
Ministering to Ministers
The Clergy Health Initiative at Duke University helps pastors find strength amid stress.
November 3, 2023 | Duke University Magazine









