Challenge
Neither North Carolina nor South Carolina has expanded its Medicaid program in response to the 2010 Affordable Care Act. As a result, uninsured rates — and risks — are much higher than other states.
Neither North Carolina nor South Carolina has expanded its Medicaid program in response to the 2010 Affordable Care Act. As a result, uninsured rates — and risks — are much higher than other states.
Supported by funding from The Duke Endowment, the AccessHealth Initiative launched in 2008 to reduce health disparities, improve clinical outcomes, decrease avoidable hospital use and expand access to care among low-income, uninsured adults throughout the Carolinas.
This support has led to large numbers of adults being enrolled, significant amounts of care being donated by physicians and hospitals, and an overall decline in risk factors in participating adults
The use of virtual care technology and patient home visits by network staff are all contributing to positive outcomes.
Studies have shown that uninsured people receive less medical care, less timely care and have worse health outcomes. Their lack of insurance coverage is not only a financial burden, it is connected to about 18,000 extra deaths per year among adults. In the Carolinas, the number of uninsured adults has increased significantly due to COVID-related job losses, bringing the collective uninsured rate from 16 percent to 20 percent. Other states have addressed this challenge by expanding their Medicaid programs to cover low-income adults through a provision in the 2010 Affordable Care Act. So far, neither North Carolina nor South Carolina has expanded its Medicaid program.

The AccessHealth Initiative launched in 2008 to reduce health disparities, improve clinical outcomes, decrease avoidable hospital use and expand access to care among low-income, uninsured adults. Components of the health care safety net have been organized into integrated provider networks to help this vulnerable population receive a continuum of services. The Duke Endowment funds 30 AccessHealth networks across the Carolinas, with 18 in North Carolina and 12 in South Carolina.
These networks identify vulnerable adults who need a medical home, assigns them to a primary care provider and then supports them with care navigation. A core tenet of this initiative is provider volunteerism, where the networks recruit physicians and hospitals to participate.
State implementation teams housed in the Carolinas Health Innovation Institute help the networks with planning and implementation, identifying and understanding best practices, and facilitating group learning. The networks report evaluation metrics through a two-state data portal that helps them understand their impact. The data is used to produce comparative reports that help identify best practices and opportunities for improvement.
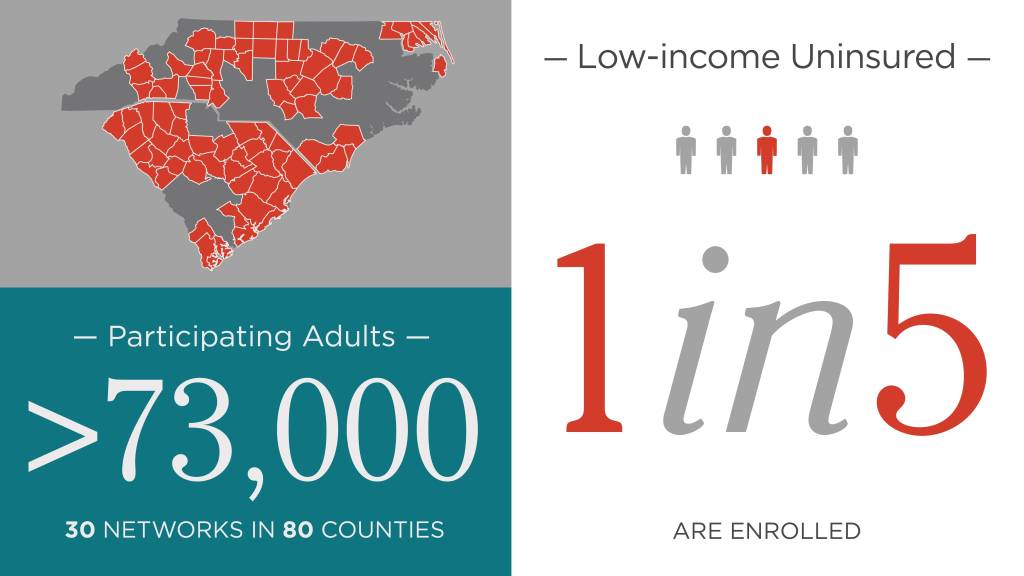
More than 73,000 adults are enrolled in the 30 networks, which span 80 counties across the two states. Over the past year, the value of medical services donated by participating physicians and hospitals totaled $582 million; some $78 million in hospital costs were avoided. Early trends also show an overall decline of the percentage of diabetic patients with an elevated blood sugar level.
Most of the 30 networks have community health workers on staff who visit patients in their homes to address challenges with leading a healthy life, and to facilitate compliance with a treatment plan as prescribed by their primary care provider. Community health workers focus on the social determinants of health, develop trusting relationships with patients and help reach marginalized individuals. Studies of minority populations with interventions by community health workers have shown improved blood sugar levels for diabetic patients and a reduction in unnecessary emergency room visits.
During COVID-19, the networks learned how to incorporate virtual processes into their work. For example, the networks are facilitating virtual visits between providers and AccessHealth patients, and they are offering a virtual enrollment process for eligible adults. Technology has become an important tool as the networks navigate these new challenges, and the state implementation teams are helping them understand and apply best practices.
