News
Endowment Intends to Distribute Up to $5B Over 15 Years
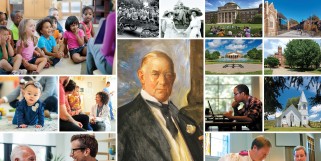
December 10, 2024 | The Duke Endowment
The Duke Endowment’s Trustees announced their intent to distribute up to $5 billion in grants across North Carolina and South Carolina over the next 15 years.
Latest News & Stories
Get the latest from the Endowment and read more about the impact of the work being done by our grantees and individuals in the field
News


Duke Endowment intends to award up to $5 billion over 15 years
The Duke Endowment will distribute up to $5 billion in grants over 15 years across North Carolina and South Carolina.
December 18, 2024 | Philanthropy News Digest